Abstract
Throughout much of the world, 'race' and 'ethnicity' are key determinants of health. For example, African Americans have, by some estimates, a twofold higher incidence of fatal heart attacks and a 10% higher incidence of cancer1,2 than European Americans, and South Asian– or Caribbean-born British are ∼3.5 times as likely to die as a direct result of diabetes than are British of European ancestry3. The health care that people receive also depends on 'race' and 'ethnicity'. African Americans are less likely to receive cancer-screening services and more likely to have late-stage cancer when diagnosed2 than European Americans. Health disparities such as these are one of the greatest social injustices in the developed world and one of the most important scientific and political challenges.
Similar content being viewed by others
Main
Most current health disparities have little or perhaps nothing to do with genetics, depending instead on socioeconomic and other environmental factors4, including inequalities in the delivery of health care. But this fact should not make us reject the possibility that biological differences associated with 'race' or 'ethnicity' will contribute to disparities in the future. Substantial changes are occurring in how medicines are developed and how they are used, and some of these changes present risks that medicines will become less inclusive. Some of the variation in how medicines work may correlate with racial or ethnic groups, exacerbating health disparities. Here we review ways in which genetics could contribute to future health disparities and outline some general research approaches that could counter this.
Why might medicines become less inclusive?
Advances in genetic technologies should improve our understanding of disease etiology and of the factors influencing response to treatment5. Although there has been relatively little progress to date in using genetics to improve the treatment of common diseases, there are some encouraging signs of progress in basic research6,7,8. If genetics does eventually prove relevant to the treatment of common diseases, then to the extent that genetic advances are uneven among racial and ethnic groups, disparities may result. Perhaps the most immediate concerns about the clinical use of genetics involve pharmacogenetics, which seeks to identify the genetic factors that influence responses to medicines. Studying drug response might be more clinically useful than studying disease predispostion6,9, at least in the near term. Pharmacogenetics also seems poised to become a common component of the drug-development pipeline10, with proof-of-concept studies having demonstrated its potential11. For these reasons, we focus this perspective on pharmacogenetics.
For convenience of presentation, we shall not attempt to define 'race' or 'ethnicity' here. Our primary aim is to discuss the evidence for differences among groups, and so we consider mainly how people are distinguished in the current medical literature, for example, in clinical trials; therefore, we refer to different groups as 'racial' or 'ethnic' groups. We do, however, briefly review debates about the extent to which human genetic structure correlates with racial or ethnic groupings.
The influence of race or ethnicity on the efficacy and safety of existing medicines may guide our expectations for the future. Therefore, we begin with a review of evidence concerning whether specific drugs work differently in different racial or ethnic groups. The concerns about how genetics might influence the inclusiveness of medicines can be broadly divided into three partially overlapping categories: (i) pharmacogenetic diagnostics, in which individual genotype is used to guide the selection of medicines; (ii) molecular subclassification of disease, in which genetic features of a disease are used to guide the choice of therapy; and (iii) pipeline pharmacogenetics, in which genetics is used during the evaluation of new chemical entities.
Inclusiveness of current medicines
At least 29 medicines (or combinations of medicines) have been claimed, in peer-reviewed scientific or medical journals, to have differences in either safety or, more commonly, efficacy among racial or ethnic groups (Table 1). But these claims are universally controversial12,13,14, and there is no consensus on how important race or ethnicity is in determining drug response.
Nevertheless, from 1995 to 1998, the labels of 8% of new drug products (15 of 185) contained a statement about racial or ethnic differences in effectiveness15. For an overview of the relationship between racial or ethnic group and drug response, we compiled a list of drugs claimed to have different effects in different racial or ethnic groups on the basis of reviews16 and PubMed literature searches using combinations of the following key words and phrases: ethnic*, race, racial, drug response, pharmacokinetic*, cytochrome P450. We also determined whether there is any evidence for a genetic or a physiological contribution to the reported racial or ethnic differences in drug response, or any other evidence that the differences are real. In cases where the differences in response are associated with underlying physiological differences (as in the case of angiotensin I–converting enzyme (ACE) inhibitors), these physiological differences may be influenced by environment, genetics or both. Genetic epidemiology methods, including migrant studies, studies of admixed populations and comparisons of populations in different geographical locations (e.g., West Africans and African Americans), can be used to assess the basis of racial or ethnic differences in response to drugs17. The most direct way to assess differences in drug response among racial or ethnic groups is to find the causes of the variable drug response and investigate how these causes differ among the groups. In most cases, however, the genetic bases of variable drug responses are too poorly known to allow a direct assessment. The one exception is beta-blockers: a polymorphism in the drug target may contribute to the differences in responses.
Many studies of drug response are small, and study designs vary. There is also a bias towards studies comparing European Americans and African Americans, reflecting a focus on the American racial or ethnic context. Certain therapeutic areas are particularly prominent among the list of medicines, most notably those related to cardiovascular disease. For example, there is arguably a consensus in the literature that African Americans respond less well than European Americans to beta-blockers, ACE inhibitors and angiotensin-receptor blockers, some of the main agents now used to treat heart-related conditions. Conversely, African Americans may respond as well as or better than European Americans to diuretics and calcium-channel blockers.
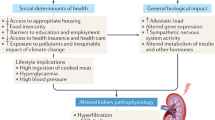
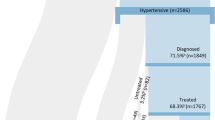
Some have argued that these differences result from underlying differences in the causes of hypertension in individuals of (west) African ancestry and of European ancestry18. For example, European American and African American hypertensive individuals typically differ in characteristics such as salt sensitivity, plasma volume and renin levels19; there could be differences in the pathogenesis of hypertension. Decreased sensitivity to beta-blockers might be associated with the higher proportion of low-renin hypertension found in African Americans, and nonadrenergic mechanisms might contribute more to blood pressure maintenance in African Americans than in European Americans20.
Differences in response to ACE inhibitors may be related to lower bioactivity of endogenous nitric oxide in African Americans than in European Americans21. The increased benefit of treatment with nitrates and hydralazine in African Americans is consistent with this hypothesis. For example, BiDil, a drug that combines isosorbide dinitrate (a nitric oxide donor) and hydralazine (a vasodilator agent), was not sufficiently effective in treating congestive heart failure in two large, ethnically mixed clinical trials22,23 to win regulatory approval. A retrospective analysis of the original trials, however, indicated that the drug was more effective in treating the African American than the European American participants in the trial24. On that basis the US Food and Drug Administration approved a trial of BiDil in African Americans25. The trial recently terminated early because interim analyses showed the drug to be highly effective, and the makers of BiDil will now seek approval for its use in the African American population. But any genetic basis to the difference in nitric oxide bioactivity between African Americans and European Americans remains to be elucidated. Furthermore, there have been no comparative studies investigating differences in nitric oxide bioactivity between Africans and African Americans, and any relationship between endothelial nitric oxide synthase variants and plasma nitric oxide levels or other intermediate or clinical phenotypes is not fully understood26.
Genetics probably contributes to some of these reported differences between different racial or ethnic groups. On the other hand, at least some of the differences can be attributed to confounded environmental factors.
A recent study investigated blood pressure response to quinapril, an ACE inhibitor, in 533 African Americans and 2,046 European Americans with hypertension. African Americans had a lower average response to quinapril than European Americans, but age, gender, body size and pretreatment blood pressure significantly predicted blood pressure response27. These factors correlate with race or ethnicity, and when they are accounted for, the effect attributable to race or ethnicity is reduced.
Some claims for differences among racial or ethnic groups in drug response will be false positives, and these may be more likely to be reported than a negative finding28. The blood pressure response analysis makes the point that, even for real differences, it is not clear which differences (if any) are due to genetic factors and which are due to environmental correlates with race or ethnicity. The analysis also shows that there is substantial variation within racial or ethnic groups in environmental correlates of response, as will also be the case for genetic factors.
Genetic contributions to differences in drug response
In discussing possible genetic factors, it is useful to distinguish genetic factors that are specific to the drug used from those that influence the nature of the condition itself. Drug-specific effects include both pharmacokinetics (e.g., drug-metabolizing enzymes (DMEs) and transporters) and pharmacodynamics (e.g., drug targets and target-related proteins, which are often not involved in disease etiology) of the drug.
For both the disease-associated and the drug-specific effects, there is scope for intergroup differences; many pharmacogenetic variants known to influence drug response show frequency differences among racial or ethnic groups6. For example, the beta-1 adrenoceptor Arg389 variant, associated with increased response to beta-blockers29,30, is less common in African Americans than in European Americans (frequencies of 0.575 and 0.723, respectively). Many DME variants also vary in frequency among populations31, and for some DMEs (e.g., CYP2D6, CYP2C19, CYP2C9 and NAT2) the proportion of individuals with little or no functional enzyme varies substantially among populations. As a relatively benign example, because they carry null alleles of CYP2D6, up to 10% of individuals of north European ancestry experience no analgesic effect from the prodrug codeine32, whereas 98% of the inhabitants of the Arabian peninsula are able to transform codeine into the active form morphine33.
These examples show that gene variants that causally influence how individuals respond to treatment often have important differences in frequency among racial or ethnic groups. This suggests that genetic differences among racial or ethnic groups will often lead to differences in drug response. The examples we selected are consistent with the general pattern for variants known to influence drug response. Of 42 genetic variants that have been associated with drug response in two or more studies, more than two-thirds have significant differences in frequency between people of European ancestry and people of African ancestry. The average frequency difference for all 42 variants is 0.15, and nearly one-third of the variants have frequency differences greater than 0.2 (ref. 6). Many of the differences in drug response among racial or ethnic groups reported in Table 1 are therefore expected to be influenced to some degree by genetics. These differences will often be modest and may not be clinically significant, but we must expect that such differences will exist and will be partially genetic.
Overall, analyses of responses to existing medicines and new chemical entities are far from conclusive about the scope for genetic differences among groups to contribute to variable drug response. In most cases it is difficult to separate genetic from environmental factors. For example, one study found significant differences in response to treatment of childhood acute lymphoblastic leukemia among racial or ethnic groups, with greatest response in Asians, followed by Europeans, Hispanics and African Americans34. Other investigators, however, found no difference in outcome when African Americans and Europeans Americans were given equal access to the most advanced therapies35. It was suggested that the conflicting findings were “possibly due to the specialized referral base of the unique practice of St Jude's Hospital [where the latter study took place], which attracts patients from an 8-state area and provides therapy at no cost to the patient's family”34. Nevertheless, there are gene variants that influence drug response that differ among racial or ethnic groups. It is therefore impossible to rule out the existence of such variation, as some investigators seem to have implied. For example, Cooper et al. stated, “Race-specific therapy draws its rationale from the presumption that the frequencies of genetic variants influencing the efficacy of the drug are substantially different among races. This result is hard to demonstrate for any class of drugs, including those used to treat heart failure”12. First, therapeutic response may differ among racial or ethnic groups either because of average genetic or environmental differences. Thus, race-specific therapy does not draw its rationale from a presumption of genetic differences. In the case of BiDil, it is not currently known whether it works differently in African Americans and European Americans because of genetics, environment or both. Second, there is no shortage of gene variants known to influence drug response that have substantial differences in frequency among racial or ethnic groups.
Despite the limited information currently available, we can draw three general conclusions about genetic contributions to differences in drug response. First, genetic differences among groups are graded, as opposed to dichotomous. Second, when genetic factors have a role, identifying the genetic factors themselves so that they can be considered directly will reduce the need to consider race or ethnicity as a loose proxy for predicting drug response. For example, we noted that most individuals from the Arabian Peninsula would respond to codeine, whereas up to 10% of North Europeans would not. A simple genetic test would indicate who would respond, regardless of geographic ancestry. Third, many differences in drug response associated with race or ethnicity are due to environmental correlates rather than population genetic differences. This implies that even when the genetic structure of a test population is taken into account, it may still be appropriate to consider race or ethnicity as a variable in order to take account of the environmental correlations17.
Pharmacogenetic diagnostics
One common view of the role of pharmacogenetics is that it should provide diagnostic analyses that allow matching of medicines with the genetic makeup of an individual, to ensure use of medicines most likely to be effective and least likely to produce adverse drug reactions (ADRs). This role of pharmacogenetics is best exemplified by a diagnostic test for low-activity variants of the gene TPMT, which encodes an enzyme that metabolizes thiopurines, which are used to treat acute lymphoblastic leukemia, rheumatoid arthritis and inflammatory bowel disease36. Individuals with intermediate or deficient activity (partially predictable from TPMT genotype) risk toxicity at standard doses and must take smaller doses. Another example is the ALOX5 promoter polymorphism. Here, genotype predicts response to leukotriene receptor antagonists37. Individuals without leukotriene activity will not respond as well. Unlike the TPMT diagnostic test, this analysis is not currently used in the clinic, probably because nonresponders do not suffer adverse effects from an ineffective drug.
For pharmacogenetic diagnostics to be useful, they must be sufficiently specific and sensitive. This will be a difficult challenge. The predictive values of pharmacogenetic tests will often be low38, whereas prediction of an ADR, for example, may have very stringent requirements. Ideally, a test for an ADR will have high positive and negative predictive values (the proportion of people with a positive test who will experience an ADR when the drug is administered and the proportion of people with a negative test who will not have an ADR, respectively). For a severe ADR, a high negative predictive value is essential. In some cases, however, positive predictive value will also be important, for example, when alternative medicines are available. Unless there is a high positive predictive value, many individuals will be misclassified as likely to have the ADR and therefore may not get the best treatment.
Will pharmacogenetic tests be equally predictive across different ethnic groups? There are two different reasons why a diagnostic test might perform differently among racial or ethnic groups. The first and most fundamental reason is that underlying physiology may differ among racial or ethnic groups. For example, the variant that influences response to a drug in one racial or ethnic group might not have the same effect, on average, in another group because of different gene-gene or gene-environment interactions. For example, the 3435C→T polymorphism in ABCB1 has been variably associated with altered drug response39,40, pharmacokinetics and P-glycoprotein expression41, but the correlation between the polymorphism and P-glycoprotein levels is not consistent across ethnic groups42,43. If 3435C→T is the causal polymorphism (and this has not been proven), then this could be an example of physiological differences across ethnic groups. The second, and perhaps more likely, reason is that the diagnostic test uses a proxy, for example, if it is based on linkage disequilibrium (LD). LD is the nonrandom association of alleles at different polymorphic sites in the genome, and levels are often high across long genomic stretches, making it hard to know whether an associated variant is causal or just a marker for (i.e., usually inherited with) the causal variant. The predictive value of an LD diagnostic test will depend on the degree of association between the markers and the underlying causal variants, and there is considerable variation in the pattern of LD among populations44. Unfortunately, diagnostic tests that are based on markers serving as proxies for the causal variants will generally have different predictive properties among different racial or ethnic groups.
One recent example provides a stark warning about the applicability of diagnostic tests across racial or ethnic groups. Abacavir is an effective antiretroviral drug used to treat HIV-1 infection. Approximately 5% of people treated with Abacavir develop a hypersensitivity reaction that requires them to stop taking the drug. Pharmacogenetic studies have identified multiple markers in the human leukocyte antigen (HLA)-B chromosomal region, including HLA-B*5701, that are associated with hypersensitivity to Abacavir in European Americans45,46,47 but not in African Americans46. Therefore, a pharmacogenetic diagnostic test using this allele would have no predictive value in African Americans. In this case, it is not clear whether Abacavir hypersensitivity has different underlying causes in African Americans versus European Americans. The HLA-B alleles are situated in a tract of ∼∼200 kb with extensive LD, and is not clear which variants within this tract are responsible for the association in Europeans and Hispanics. Considerably larger association studies or functional studies will be required to determine whether the HLA-B*5701 allele or an associated variant is responsible for the ADR.
These considerations also suggest that in the near term at least, pharmacogenetic diagnostics should rely on validated causal variants rather than either single markers as proxies or genome-wide SNP profiles, both of which will usually rely on LD to generate associations between the markers and the drug responses. Because the degree and pattern of LD typically vary among populations, LD marker-based tests will often need to be adjusted for different racial or ethnic groups. This requires large, expensive studies of many populations.
Genetic subclassification of disease
Common diseases result from complex interactions between genetic and environmental factors. As more is learned about the genetic bases of common diseases, such diseases may be divided into distinct subclasses with similar phenotypes but different underlying genetic bases. In many cases, specific drugs are indicated for specific subtypes of a disease: for example, Herceptin is indicated for the subpopulation of individuals with breast cancer who express ERBB2, and Gleevec is indicated for individuals with chronic myeloid leukemia resulting from the BCR-ABL1 gene fusion. Similarly, two recent studies identified mutations in EGFR in lung cancers, which predict response to the tyrosine kinase inhibitor gefitinib (also known by the trade name Iressa)48,49.
It is unclear how often the underlying genetic bases of disease differ among racial or ethnic groups, but this may occur for some diseases. For example, susceptibility to Crohn disease is associated with three polymorphisms in CARD15 in European Americans8, but none of these variants was present in a sample of Japanese individuals with Crohn disease50. Another example is a CCR5 variant that protects against HIV infection and progression. Up to 25% of European Americans are heterozygous with respect to this variant, but it is practically absent in other ethnic groups51. The EGFR mutations that predict response to gefitinib are more frequent in Japanese individuals, possibly explaining their increased responsiveness.
Even when a genetic variant associated with disease susceptibility is present in multiple ethnic groups, it may have different effects. For example the E4 variant of APOE is associated with a substantially increased risk of Alzheimer disease52, which varies among racial or ethnic groups. Homozygosity with respect to the E4 allele increases the risk of Alzheimer disease by a factor of 33 in Japanese, 15 in European Americans and 6 in African Americans53. A more recent study also found differential effects of the E4 allele between Europeans Americans and African Americans54. It is impossible to determine from current evidence whether these differences reflect an interaction of APOE with genetic background or with environment.
To the extent that progress in understanding the genetic bases of common disease is faster in some ethnic groups than in others, the ability to genetically subclassify diseases might proceed faster in some groups than others, meaning that treatment can be made more precise in these groups. In this context, it may be a concern that the HapMap project is not sufficiently inclusive.
The HapMap Project is an international research effort to describe the common patterns of human genetic variation in order to facilitate future studies that relate genetic variation to health and disease. The project currently includes European Americans, Africans (the Yoruba in Ibadan, Nigeria), Japanese and Han Chinese but excludes Native Americans and Pacific Islanders, two of the five racial categories indicated by the US Food and Drug Administration and argued by some to be the principal determinants of the geographic component of human genetic variation17. Exclusion of Native Americans in particular seems inconsistent with the policy of the US National Institutes of Health to include minorities in biomedical research (there ∼4.3 million Native Americans or Native Americans in combination with one or more other races in the US, making up 1.5% of the total population; http://www.census.gov/Press-Release/www/releases/archives/facts_for_features/001492.html). The decision to exclude Native Americans was made after consultation with some representatives of the Native American health research community, who cited concerns about HapMap data being used to facilitate population history studies and comparisons among populations55. In a broader sense, given the genetic diversity among African populations, it would almost certainly have been more informative to choose a second African population as opposed to a second East Asian one.
Drug pipeline pharmacogenetics
In some ways the use of pharmacogenetics during the development of potential new therapies generates the most serious concerns because of its potential to influence the medicines that are brought to market. In the past, the basic model in drug development was to find drugs that are as widely applicable as possible, hence the effort to prove efficacy in large, expensive phase 3 trials. Now there is interest in carrying out smaller, less expensive trials using genetics56. Although the idea of focusing clinical trials on subgroups of individuals is not new, as stratification by disease subtype has always been a goal of medical research57, the use of genetics in this context is new. Pharmaceutical companies have long tended, when possible, not to pursue compounds known to be metabolized largely by highly polymorphic systems, such as CYP2D6, but pharmacogenetics has otherwise had a small role in drug development. Increasingly, however, there is interest in the use of systematic genetic analyses to identify the genetic causes of variable responses during the evaluation of new chemical entities. Widespread use of such reverse genetic strategies could result in important changes in drug development, including reliance on more focused clinical trials56.
Early identification of a marker for drug response could lead to smaller phase 3 trials involving those individuals who are more likely to respond. Efficacy pharmacogenetics might lower the cost of phase 3 clinical trials if randomization could be applied to a population of individuals in whom the drug is effective selected in phase 2 trials56. This would result in individuals with unfavorable genetic profiles being excluded from trials, even though a proportion of them would probably respond to the drug (albeit less frequently than the target population). There is a risk of creating 'orphan genotypes' that are left untreated for either scientific (difficult to treat) or economic (too small to be economically viable) reasons. Many genetic variants, including DME polymorphisms and drug target polymorphisms, vary in frequency among populations. If a marker for efficacy has low prevalence in a certain ethnic population, that population may be excluded from research or treatment.
How to represent human population genetic structure
It is difficult to address concerns about differences among racial or ethnic groups if there is no agreement about what constitutes a group. This is a contentious issue, and there seems to be little hope the community will soon reach a consensus14,17. It may be helpful, therefore, to begin with some areas of general agreement. Most importantly, no matter how groups are defined, most of the genetic variation in the species is due to differences among individuals within groups, not to differences between groups. It is also agreed, however, that individuals with the same geographic ancestry are more similar, on average, than individuals with different geographic ancestries.
The main areas of dispute are how to represent that portion of our overall variability that does correlate with geography, and how important this portion of our variation is in medicine. Risch and colleagues17 proposed using five racial groups in biomedical research based on continental ancestry. Although this method is easy to implement, it is unclear how well it captures human population structure. A second method, called explicit genetic inference, ignores geographic, racial or ethnic labels and instead groups similar individuals using genetic data58. There has been debate about how well self-identified ethnicity corresponds with explicit genetic inference and, more generally, how well we understand the global pattern of human genetic diversity17,58. Our view is that worldwide patterns of genetic variation are not well known. Data from Rosenberg and colleagues seem to support the scheme proposed by Risch and colleagues of a small number of groups corresponding largely to continent of origin; in a sample of 1,056 individuals from 52 populations they identified six main genetic clusters, five of which correspond to geographic regions59. Although the sample set they used is referred to as a 'diversity panel', geographic sampling is far from comprehensive. The results would be far more graded between groupings, and the groupings themselves might fade or multiply, if more comprehensive samples were analyzed.
Even when there is a generally good correspondence between self-identified ethnicity and explicit genetic inference, we believe that there are contexts where it is still advisable to obtain the most precise information possible about genetic structure. For example, in evaluating new medicines, it would be straightforward to include explicit genetic inference as part of the overall analyses, with a negligible increase in cost and complexity. Groups identified by ethnic or racial labels (or genetics) may themselves be internally structured genetically. This structure would be hard to represent with ethnic labels but is straightforward to represent using genetic inference. For example, estimates of the proportion of European ancestry in African Americans average ∼21%, but there is a wide range of ancestry proportions among individuals60.
The importance of group differences in medical genetics has been the subject of much debate. Cooper and colleagues argue that race is not an adequate proxy for choosing a drug12. Although it is true that individual genotype will always be more informative than racial or ethnic labels (for genetic effects), we believe that in some cases, race and ethnicity may be useful biological proxies for the underlying genetic variation. There are many examples of variants that are known to influence drug response and that differ substantially among racial or ethnic groups. Because there are many other variants that are not known, some drug response will correlate with racial or ethnic groups, some of which may be relevant to the selection of treatment alternatives. This source of genetic variation can and should be represented during our period of ignorance of the underlying causal factors. In some settings, this may be best done by explicit genetic inference (e.g., during the evaluation of new medicines), whereas in other settings, self-identified racial or ethnic labels may need to suffice (e.g., routine clinical practice, where explicit genetic inference is not currently practical).
Conclusions
Our aim was to outline how advances in genetics could contribute, even if modestly, to disparities in the quality of health care among different racial or ethnic groups. To the extent that this is agreed to be a serious concern, the solution is straightforward: more and better research in those groups that have been traditionally under-represented in clinical and other biomedical studies. The US National Institutes of Health specifically requires “members of minority groups and their subpopulations must be included in all NIH-supported biomedical and behavioral research projects involving human subjects” (http://grants2.nih.gov/grants/policy/emprograms /overview/women-and-mi.htm). In this spirit, Francis Collins, the director of the US National Human Genome Research Institute, recently outlined a case for a large-scale prospective cohort study in the US to identify genetic and environmental influences on disease, and specifically called for oversampling in ethnic minority groups61. Similar European efforts have, however, simply ignored the issue. The UK Biobank project (http://www.ukbiobank.ac.uk/), for example, is sampling minorities in proportion to their representation. This effectively excludes minorities, as the numbers collected will be too small to allow identification of gene-environment interactions specific to the minority groups. We would like to see this decision reconsidered. We welcome the recent proposal from Howard University to begin the Genomic Research in the African Diaspora, which aims to identify and characterize genetic polymorphisms in African Americans and their ancestral populations (http://www.genomecenter.howard.edu/intro.htm).
More specifically, it is important to carry out basic pharmacogenetics research in as broad a range of ethnic groups as possible. It is nevertheless inevitable that diagnostic tests will often be identified in specific ethnic groups, and in these cases, it is essential that the diagnostic be tested explicitly in other ethnic groups, as scientists from GlaxoSmithKline did with Abacavir46. In this context, one valuable tool may be the use of healthy volunteers in those cases where drugs can be safely administered, or where probe drugs may indicate the effect of a gene variant on transport or metabolism. The use of healthy volunteers would also facilitate efforts to ensure that functional variation at relevant genes is equally well described in all racial or ethnic groups. Finally, even greater efforts are required to expand the diversity of drug trial populations. The results of such trials could also be interpreted with more clarity, and the effects of genetic structure more systematically assessed, if genetic structure were routinely analyzed in drug trials58.
Overall, it is difficult to say whether advances in genomic medicine will exacerbate or attenuate health disparities. It seems that no matter how research is done, most medicines will tend to work similarly among different human populations. Because of our youth as a species, most human genetic variation comes from an ancestral source population and is present in most current racial or ethnic groups. But rough statistical similarity in how medicines work among racial or ethnic groups is not always good enough. For example, in the American context, it is both morally and politically unacceptable for the public and private sectors to follow a research agenda leading to medicines that are 5% more effective in European Americans than in African Americans. This sort of an outcome is possible unless there are more explicit efforts are made to ensure that medicines are inclusive.
References
Robertson, J.A. Constitutional issues in the use of pharmacogenomic variations associated with race. in Pharmacogenomics: Social, Ethical and Clinical Dimensions 291–316 (Wiley-Liss, 2003).
Agency for Healthcare Research and Quality. National Healthcare Disparities Report (Agency for Healthcare Research and Quality).
London Health Observatory. Ethnic Disparities in Health and Health Care: A Focused Review of the Evidence and Selected Examples of Good Practice (London Health Observatory, 2004).
Cooper, R.S. Social inequality, ethnicity and cardiovascular disease. Int. J. Epidemiol. 30 Suppl 1, S48–S52 (2001).
Collins, F.S., Green, E.D., Guttmacher, A.E. & Guyer, M.S. A vision for the future of genomics research. Nature 422, 835–847 (2003).
Goldstein, D.B., Tate, S.K. & Sisodiya, S.M. Pharmacogenetics goes genomic. Nat. Rev. Genet. 4, 937–947 (2003).
Laitinen, T. et al. Characterization of a common susceptibility locus for asthma-related traits. Science 304, 300–304 (2004).
Hugot, J.P. et al. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn's disease. Nature 411, 599–603 (2001).
Schmith, V.D. et al. Pharmacogenetics and disease genetics of complex diseases. Cell Mol. Life Sci. 60, 1636–1646 (2003).
Food and Drug Administration. Guideline for Industry Pharmacogenomic Data Submissions (Food and Drug Administration, 2004).
Danoff, T.M. et al. A Gilbert's syndrome UGT1A1 variant confers susceptibility to tranilast-induced hyperbilirubinemia. Pharmacogenomics J. 4, 49–53 (2004).
Cooper, R.S., Kaufman, J.S. & Ward, R. Race and genomics. N. Engl. J. Med. 348, 1166–1170 (2003).
Burchard, E.G. et al. The importance of race and ethnic background in biomedical research and clinical practice. N. Engl. J. Med. 348, 1170–1175 (2003).
Schwartz, R.S. Racial profiling in medical research. N. Engl. J. Med. 344, 1392–1393 (2001).
Evelyn, B. et al. Participation of racial/ethnic groups in clinical trials and race-related labeling: a review of new molecular entities approved 1995-1999. J. Natl. Med. Assoc. 93, 18S–24S (2001).
Bjornsson, T.D. et al. A review and assessment of potential sources of ethnic differences in drug responsiveness. J. Clin. Pharmacol. 43, 943–967 (2003).
Risch, N., Burchard, E., Ziv, E. & Tang, H. Categorization of humans in biomedical research: genes, race and disease. Genome Biol. 3, comment2007 (2002).
Ferdinand, K.C. Recommendations for the management of special populations: racial and ethnic populations. Am. J. Hypertens. 16, 50S–54S (2003).
Saunders, E. Hypertension in blacks. Prim. Care 18, 607–622 (1991).
Lang, C.C. et al. Blunted blood pressure response to central sympathoinhibition in normotensive blacks: increased importance of nonsympathetic factors in blood pressure maintenance in blacks. Hypertension 30, 157–162 (1997).
Kalinowski, L., Dobrucki, I.T. & Malinski, T. Race-specific differences in endothelial function: predisposition of African Americans to vascular diseases. Circulation 109, 2511–2517 (2004).
Cohn, J.N. et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure. Results of a Veterans Administration Cooperative Study. N. Engl. J. Med. 314, 1547–1552 (1986).
Cohn, J.N. et al. A comparison of enalapril with hydralazine-isosorbide dinitrate in the treatment of chronic congestive heart failure. N. Engl. J. Med. 325, 303–310 (1991).
Carson, P., Ziesche, S., Johnson, G. & Cohn, J.N. Racial differences in response to therapy for heart failure: analysis of the vasodilator-heart failure trials. Vasodilator-Heart Failure Trial Study Group. J. Card. Fail. 5, 178–187 (1999).
Kahn, J. How a drug becomes “ethnic”: law, commerce, and the production of racial categories in medicine. Yale J. Health Policy Law Ethics 4, 1–46 (2004).
Li, R. et al. Relation of endothelial nitric oxide synthase gene to plasma nitric oxide level, endothelial function, and blood pressure in African Americans. Am. J. Hypertens. 17, 560–567 (2004).
Mokwe, E. et al. Determinants of blood pressure response to quinapril in black and white hypertensive patients: the Quinapril Titration Interval Management Evaluation trial. Hypertension 43, 1202–1207 (2004).
Lohmueller, K.E., Pearce, C.L., Pike, M., Lander, E.S. & Hirschhorn, J.N. Meta-analysis of genetic association studies supports a contribution of common variants to susceptibility to common disease. Nat. Genet. 33, 177–182 (2003).
Sofowora, G.G. et al. A common beta1-adrenergic receptor polymorphism (Arg389Gly) affects blood pressure response to beta-blockade. Clin. Pharmacol. Ther. 73, 366–371 (2003).
Johnson, J.A. et al. Beta 1-adrenergic receptor polymorphisms and antihypertensive response to metoprolol. Clin. Pharmacol. Ther. 74, 44–52 (2003).
Xie, H.G., Kim, R.B., Wood, A.J. & Stein, C.M. Molecular basis of ethnic differences in drug disposition and response. Annu. Rev. Pharmacol. Toxicol. 41, 815–850 (2001).
Bradford, L.D. CYP2D6 allele frequency in European Caucasians, Asians, Africans and their descendants. Pharmacogenomics 3, 229–243 (2002).
McLellan, R.A., Oscarson, M., Seidegard, J., Evans, D.A. & Ingelman-Sundberg, M. Frequent occurrence of CYP2D6 gene duplication in Saudi Arabians. Pharmacogenetics 7, 187–191 (1997).
Kadan-Lottick, N.S., Ness, K.K., Bhatia, S. & Gurney, J.G. Survival variability by race and ethnicity in childhood acute lymphoblastic leukemia. JAMA 290, 2008–2014 (2003).
Pui, C.H. et al. Results of therapy for acute lymphoblastic leukemia in black and white children. JAMA 290, 2001–2007 (2003).
McLeod, H.L. & Siva, C. The thiopurine S-methyltransferase gene locus — implications for clinical pharmacogenomics. Pharmacogenomics 3, 89–98 (2002).
Drazen, J.M. et al. Pharmacogenetic association between ALOX5 promoter genotype and the response to anti-asthma treatment. Nat. Genet. 22, 168–170 (1999).
Holtzman, N.A. Clinical Utility of pharmacogenetics and pharmacogenomics. in Pharmacogenomics: Social, Ethical and Clinical Dimensions 163–185 (Wiley-Liss, 2003).
Siddiqui, A. et al. Association of multidrug resistance in epilepsy with a polymorphism in the drug-transporter gene ABCB1. N. Engl. J. Med. 348, 1442–1448 (2003).
Fellay, J. et al. Response to antiretroviral treatment in HIV-1-infected individuals with allelic variants of the multidrug resistance transporter 1: a pharmacogenetics study. Lancet 359, 30–36 (2002).
Hoffmeyer, S. et al. Functional polymorphisms of the human multidrug-resistance gene: multiple sequence variations and correlation of one allele with P-glycoprotein expression and activity in vivo. Proc. Natl. Acad. Sci. USA 97, 3473–3478 (2000).
Oselin, K., Gerloff, T., Mrozikiewicz, P.M., Pahkla, R. & Roots, I. MDR1 polymorphisms G2677T in exon 21 and C3435T in exon 26 fail to affect rhodamine 123 efflux in peripheral blood lymphocytes. Fundam. Clin. Pharmacol. 17, 463–469 (2003).
Sakaeda, T., Nakamura, T. & Okumura, K. Pharmacogenetics of MDR1 and its impact on the pharmacokinetics and pharmacodynamics of drugs. Pharmacogenomics 4, 397–410 (2003).
Reich, D.E. et al. Linkage disequilibrium in the human genome. Nature 411, 199–204 (2001).
Hetherington, S. et al. Genetic variations in HLA-B region and hypersensitivity reactions to abacavir. Lancet 359, 1121–1122 (2002).
Hughes, A.R. et al. Association of genetic variations in HLA-B region with hypersensitivity to abacavir in some, but not all, populations. Pharmacogenomics 5, 203–211 (2004).
Mallal, S. et al. Association between presence of HLA-B*5701, HLA-DR7, and HLA-DQ3 and hypersensitivity to HIV-1 reverse-transcriptase inhibitor abacavir. Lancet 359, 727–732 (2002).
Paez, J.G. et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 304, 1497–1500 (2004).
Lynch, T.J. et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N. Engl. J. Med. 350, 2129–2139 (2004).
Yamazaki, K., Takazoe, M., Tanaka, T., Kazumori, T. & Nakamura, Y. Absence of mutation in the NOD2/CARD15 gene among 483 Japanese patients with Crohn's disease. J. Hum. Genet. 47, 469–472 (2002).
Stephens, J.C. et al. Dating the origin of the CCR5-Delta32 AIDS-resistance allele by the coalescence of haplotypes. Am. J. Hum. Genet. 62, 1507–1515 (1998).
Corder, E.H. et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer's disease in late onset families. Science 261, 921–923 (1993).
Farrer, L.A. et al. Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease. A meta-analysis. APOE and Alzheimer Disease Meta Analysis Consortium. JAMA 278, 1349–1356 (1997).
Evans, D.A. et al. Incidence of Alzheimer disease in a biracial urban community: relation to apolipoprotein E allele status. Arch. Neurol. 60, 185–189 (2003).
Integrating ethics and science in the International HapMap Project. Nat. Rev. Genet. 5, 467–475 (2004).
Roses, A.D. Genome-based pharmacogenetics and the pharmaceutical industry. Nat. Rev. Drug Discov. 1, 541–549 (2002).
Lindpaintner, K. Pharmacogenetics and the future of medical practice. J. Mol. Med. 81, 141–153 (2003).
Wilson, J.F. et al. Population genetic structure of variable drug response. Nat. Genet. 29, 265–269 (2001).
Rosenberg, N.A. et al. Genetic structure of human populations. Science 298, 2381–2385 (2002).
Smith, M.W. et al. A high-density admixture map for disease gene discovery in african americans. Am. J. Hum. Genet. 74, 1001–1013 (2004).
Collins, F.S. The case for a US prospective cohort study of genes and environment. Nature 429, 475–477 (2004).
Exner, D.V., Dries, D.L., Domanski, M.J. & Cohn, J.N. Lesser response to angiotensin-converting-enzyme inhibitor therapy in black as compared with white patients with left ventricular dysfunction. N. Engl. J. Med. 344, 1351–1357 (2001).
Weir, M.R. et al. Nocturnal reduction of blood pressure and the antihypertensive response to a diuretic or angiotensin converting enzyme inhibitor in obese hypertensive patients. TROPHY Study Group. Am. J. Hypertens. 11, 914–920 (1998).
Weir, M.R., Gray, J.M., Paster, R. & Saunders, E. Differing mechanisms of action of angiotensin-converting enzyme inhibition in black and white hypertensive patients. The Trandolapril Multicenter Study Group. Hypertension 26, 124–130 (1995).
Carson, P., Ziesche, S., Johnson, G. & Cohn, J.N. Racial differences in response to therapy for heart failure: analysis of the vasodilator-heart failure trials. Vasodilator-Heart Failure Trial Study Group. J. Card. Fail. 5, 178–187 (1999).
Stein, C.M., Lang, C.C., Nelson, R., Brown, M. & Wood, A.J. Vasodilation in black Americans: attenuated nitric oxide-mediated responses. Clin. Pharmacol. Ther. 62, 436–443 (1997).
Rosenbaum, D.A. et al. Ethnicity affects vasodilation, but not endothelial tissue plasminogen activator release, in response to bradykinin. Arterioscler. Thromb. Vasc. Biol. 22, 1023–1028 (2002).
Cubeddu, L.X. et al. A comparison of verapamil and propranolol for the initial treatment of hypertension. Racial differences in response. JAMA 256, 2214–2221 (1986).
Johnson, J.A. et al. Beta 1-adrenergic receptor polymorphisms and antihypertensive response to metoprolol. Clin. Pharmacol. Ther. 74, 44–52 (2003).
Sofowora, G.G. et al. A common beta1-adrenergic receptor polymorphism (Arg389Gly) affects blood pressure response to beta-blockade. Clin. Pharmacol. Ther. 73, 366–371 (2003).
Liu, J. et al. Gly389Arg polymorphism of beta1-adrenergic receptor is associated with the cardiovascular response to metoprolol. Clin. Pharmacol. Ther. 74, 372–379 (2003).
Xie, H.G. et al. Arg389Gly beta 1-adrenoceptor polymorphism varies in frequency among different ethnic groups but does not alter response in vivo. Pharmacogenetics 11, 191–197 (2001).
Efficacy of nadolol alone and combined with bendroflumethiazide and hydralazine for systemic hypertension. Am. J. Cardiol. 52, 1230–1237 (1983).
Friedman, B., Gray, J.M., Gross, S. & Levit, S.A. United States experience with oxprenolol in hypertension. Am. J. Cardiol. 52, 43D–48D (1983).
Beta-Blocker Evaluation of Survival Trial Investigators. A trial of the beta-blocker bucindolol in patients with advanced chronic heart failure. N. Engl. J. Med. 344, 1659–1667 (2001).
Cushman, W.C. et al. Regional and racial differences in response to antihypertensive medication use in a randomized controlled trial of men with hypertension in the United States. Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. Arch. Intern. Med. 160, 825–831 (2000).
Zanchi, A., Maillard, M. & Burnier, M. Recent clinical trials with omapatrilat: new developments. Curr. Hypertens. Rep. 5, 346–352 (2003).
Hassaballa, H., Gorelick, P.B., West, C.P., Hansen, M.D. & Adams, H.P., Jr. Ischemic stroke outcome: racial differences in the trial of danaparoid in acute stroke (TOAST). Neurology 57, 691–697 (2001).
Blann, A., Hewitt, J., Siddiqui, F. & Bareford, D. Racial background is a determinant of average warfarin dose required to maintain the INR between 2.0 and 3.0. Br. J. Haematol. 107, 207–209 (1999).
Blann, A. & Bareford, D. Ethnic background is a determinant of average warfarin dose required to maintain the INR between 3.0 and 4.5. J. Thromb. Haemost. 2, 525–526 (2004).
Taube, J., Halsall, D. & Baglin, T. Influence of cytochrome P-450 CYP2C9 polymorphisms on warfarin sensitivity and risk of over-anticoagulation in patients on long-term treatment. Blood 96, 1816–1819 (2000).
Higashi, M.K. et al. Association between CYP2C9 genetic variants and anticoagulation-related outcomes during warfarin therapy. JAMA 287, 1690–1698 (2002).
Takahashi, H. et al. Population differences in S-warfarin metabolism between CYP2C9 genotype-matched Caucasian and Japanese patients. Clin. Pharmacol. Ther. 73, 253–263 (2003).
Chapman, A.B., Schwartz, G.L., Boerwinkle, E. & Turner, S.T. Predictors of antihypertensive response to a standard dose of hydrochlorothiazide for essential hypertension. Kidney Int. 61, 1047–1055 (2002).
Aviv, A. Cellular calcium and sodium regulation, salt-sensitivity and essential hypertension in African Americans. Ethn. Health 1, 275–281 (1996).
Watkins, L.L., Dimsdale, J.E. & Ziegler, M.G. Reduced beta 2-receptor mediated vasodilation in African Americans. Life Sci. 57, 1411–1416 (1995).
Cardillo, C., Kilcoyne, C.M., Cannon, R.O. III & Panza, J.A. Attenuation of cyclic nucleotide-mediated smooth muscle relaxation in blacks as a cause of racial differences in vasodilator function. Circulation 99, 90–95 (1999).
Lang, C.C. et al. Attenuation of isoproterenol-mediated vasodilatation in blacks. N. Engl. J. Med. 333, 155–160 (1995).
Johnson, J.A., Burlew, B.S. & Stiles, R.N. Racial differences in beta-adrenoceptor-mediated responsiveness. J. Cardiovasc. Pharmacol. 25, 90–96 (1995).
Tornatore, K.M. et al. Methylprednisolone pharmacokinetics, cortisol response, and adverse effects in black and white renal transplant recipients. Transplantation 59, 729–736 (1995).
Muir, A.J., Bornstein, J.D. & Killenberg, P.G. Peginterferon alfa-2b and ribavirin for the treatment of chronic hepatitis C in blacks and non-Hispanic whites. N. Engl. J. Med. 350, 2265–2271 (2004).
Kimball, P., Elswick, R.K. & Shiffman, M. Ethnicity and cytokine production gauge response of patients with hepatitis C to interferon-alpha therapy. J. Med. Virol. 65, 510–516 (2001).
De Maria, N. et al. Impaired response to high-dose interferon treatment in African-Americans with chronic hepatitis C. Hepatogastroenterology 49, 788–792 (2002).
Netland, P.A. et al. Response to travoprost in black and nonblack patients with open-angle glaucoma or ocular hypertension. Adv. Ther. 20, 149–163 (2003).
Bhatia, S. et al. Racial and ethnic differences in survival of children with acute lymphoblastic leukemia. Blood 100, 1957–1964 (2002).
Pollock, B.H. et al. Racial differences in the survival of childhood B-precursor acute lymphoblastic leukemia: a Pediatric Oncology Group Study. J. Clin. Oncol. 18, 813–823 (2000).
Kadan-Lottick, N.S., Ness, K.K., Bhatia, S. & Gurney, J.G. Survival variability by race and ethnicity in childhood acute lymphoblastic leukemia. JAMA 290, 2008–2014 (2003).
Millward, M.J. et al. Docetaxel and carboplatin is an active regimen in advanced non-small-cell lung cancer: a phase II study in Caucasian and Asian patients. Ann. Oncol. 14, 449–454 (2003).
Goran, M.I., Bergman, R.N., Cruz, M.L. & Watanabe, R. Insulin resistance and associated compensatory responses in african-american and Hispanic children. Diabetes Care 25, 2184–2190 (2002).
Lin, K.M. et al. A longitudinal assessment of haloperidol doses and serum concentrations in Asian and Caucasian schizophrenic patients. Am. J. Psychiatry 146, 1307–1311 (1989).
Jann, M.W. et al. Haloperidol and reduced haloperidol plasma levels in Chinese vs. non-Chinese psychiatric patients. Psychiatry Res. 30, 45–52 (1989).
Matsuda, K.T. et al. Clozapine dosage, serum levels, efficacy, and side-effect profiles: a comparison of Korean-American and Caucasian patients. Psychopharmacol. Bull. 32, 253–257 (1996).
Collazo, Y., Tam, R., Sramek, J. & Herrera, J. Neuroleptic dosing in Hispanic and Asian Inpatients with schizophrenia. Mt. Sinai J. Med. 63, 310–313 (1996).
Segal, S.P., Bola, J.R. & Watson, M.A. Race, quality of care, and antipsychotic prescribing practices in psychiatric emergency services. Psychiatr. Serv. 47, 282–286 (1996).
Strakowski, S.M., Shelton, R.C. & Kolbrener, M.L. The effects of race and comorbidity on clinical diagnosis in patients with psychosis. J. Clin. Psychiatry 54, 96–102 (1993).
Chung, H., Mahler, J.C. & Kakuma, T. Racial differences in treatment of psychiatric inpatients. Psychiatr. Serv. 46, 586–591 (1995).
Walkup, J.T. et al. Patients with schizophrenia at risk for excessive antipsychotic dosing. J. Clin. Psychiatry 61, 344–348 (2000).
Zhou, H.H., Sheller, J.R., Nu, H., Wood, M. & Wood, A.J. Ethnic differences in response to morphine. Clin. Pharmacol. Ther. 54, 507–513 (1993).
Cepeda, M.S. et al. Ethnicity influences morphine pharmacokinetics and pharmacodynamics. Clin. Pharmacol. Ther. 70, 351–361 (2001).
Acknowledgements
We thank R. Cook-Deegan and C. Condit for critical reading of the manuscript. D.G. is a Wolfson / Royal Society Research Merit Award holder.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Tate, S., Goldstein, D. Will tomorrow's medicines work for everyone?. Nat Genet 36 (Suppl 11), S34–S42 (2004). https://doi.org/10.1038/ng1437
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ng1437
This article is cited by
-
Authorization of tissues from deceased patients for genetic research
Human Genetics (2018)
-
Scientometric analyses of studies on the role of innate variation in athletic performance
SpringerPlus (2014)
-
Pharmacogenetics in Primary Care: The Promise of Personalized Medicine and the Reality of Racial Profiling
Culture, Medicine, and Psychiatry (2013)
-
Pharmacogenetics of Naltrexone in Asian Americans: A Randomized Placebo-Controlled Laboratory Study
Neuropsychopharmacology (2012)
-
Genome Wide Association Study to predict severe asthma exacerbations in children using random forests classifiers
BMC Medical Genetics (2011)